Mentions of post-traumatic stress disorder (PTSD) date back to 490 B.C. when a Greek Historian named Herodotus mentioned the psychological symptoms experienced by soldiers who fought in the Battle of Marathon.
PTSD has been identified in United States history as early as the Civil War, fought from 1861-1865, and has been referred to using different terms before it became an official diagnosis in the 1970s. During World War I, it was called shell shock, while in World War II it was more common to call it battle fatigue. After the Vietnam war, it has been estimated that at least 25 percent of returning veterans have needed psychological care of some kind as a direct result of the trauma experienced by being exposed to violent warfare.
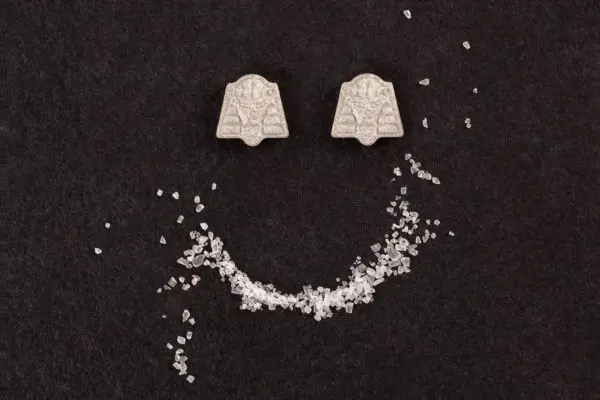
As the problem of PTSD within the community of current and former members of the military persists, it is becoming all the more imperative to improve methods of treatment. Keep reading to learn about how MDMA-assisted psychotherapy might offer a solution in the coming years.
What is PTSD?
The Department of Veterans Affairs (VA) has defined PTSD as “the development of characteristic and persistent symptoms along with difficulty functioning after exposure to a life-threatening experience or to an event that either involves a threat to life or serious injury.”
Symptoms of PTSD after combat exposure can cause lifelong suffering if left untreated (or unsuccessfully treated) and can include depression, anxiety, hypersensitivity to stimuli, nightmares, emotional detachment, cognitive and memory impairment, difficulty sleeping, and many other debilitating effects. Veterans affected by PTSD often feel disconnected from themselves and people in their lives, and lose interest in activities or communities that used to be sources of joy.
PTSD can cause chronic pain; it is estimated that anywhere from 15 to 35 percent of chronic pain patients also suffer from symptoms of PTSD. 55 to 75 percent of problematic drug or alcohol use diagnoses among veterans are comorbid with PTSD. The depressant properties of alcohol act to help suppress symptoms of PTSD, anxiety, and hypervigilance.
How does PTSD affect Veterans?
Because PTSD has a significant impact on a person’s emotions, the condition can make relationships and family life more difficult after exposure to trauma during military service. Many veterans experience difficulties with their marriages and partnerships or find it challenging to relate to their children.
PTSD might make it difficult or impossible to maintain a job, fulfill educational requirements, or hold leadership positions. Activities that may seem straightforward to a healthy individual can be an overwhelming struggle for veterans affected by PTSD, like grocery shopping or social interactions with peers.
When suffering from PTSD, many people isolate themselves to avoid experiences and people that trigger memories of traumatic events. Loneliness and estrangement only serve to deepen the painful experience of living with the condition.
Unfortunately, there is sometimes a stigma associated with mental health issues within the military community which frequently becomes a deterrent for seeking help. Those who do take action are often met with long delays to see a mental health professional in the current Veterans Affairs system, and only individuals who have been discharged on terms deemed favorable by the military are qualified to receive care. Many are fearful that seeking help for PTSD will cost them promotions their security clearance, or make them susceptible to discharge.
What is MDMA-assisted psychotherapy?
MDMA (3,4-methylenedioxymethamphetamine) is a psychoactive substance that is often referred to as ecstasy outside of the clinical setting. It produces both stimulant and mild hallucinogenic effects on the brain by influencing levels of serotonin, dopamine, norepinephrine, and oxytocin. Such neurotransmitters influence mood, energy, emotional openness, bonding, and reduce the fear response, which is elevated in those affected by symptoms of PTSD. This cocktail of neurotransmitters creates a powerful balance of motivation, relaxation, and emotional safety to face and process potentially suppressed (or repressed) painful memories, initiating the road to healing and recovery.
When used in the context of psychotherapy, MDMA can help those living with PTSD release the fear and anxiety of reliving traumatic events, thus allowing them to engage more meaningfully with the therapeutic process. MDMA is administered while a psychotherapy session occurs so that individuals can more effectively benefit during in-person treatment and become better equipped to apply cognitive-behavioral therapy practices in their daily lives afterward.
MDMA does have risks and side effects, in addition to being potentially dangerous for those with certain existing mental and physical health concerns. For more information about MDMA, its effects, and the potential risks, read Psychable’s Beginner’s Guide to MDMA.
How can MDMA-assisted psychotherapy help veterans?
The U.S. Food and Drug Administration (FDA) has designated MDMA as a Breakthrough Therapy for treating PTSD, which helps expedite reviews of clinical trials and create a more direct path to approval if the drug satisfies the requirements in trials. A study sponsored by the Multidisciplinary Association for Psychedelic Studies (MAPS) is currently in Phase 3 trials and on track to make MDMA-assisted therapy available by prescription by 2023 should it succeed.
In clinical trials so far, MDMA-assisted psychotherapy has been more effective as a treatment for PTSD than any other type of medication or psychotherapy alone. It differs from traditional methods; as opposed to medications taken daily (and possibly for the remainder of a lifetime), MDMA-assisted therapy occurs only a few times and can provide lasting effects when it is successful. In one study, more than two-thirds of participants demonstrated remission one year after treatment, no longer meeting DSM-V criteria for PTSD.
MDMA-assisted Psychotherapy is currently only available to people diagnosed with PTSD who opt to participate in studies and clinical trials, though this may change in the near future.
The harm reduction of alleviated symptoms, sometimes following just a single treatment, can provide swift relief to a community of people suffering from PTSD for whom the condition prevents ordinary function and enjoyment of life.
The possible impact of making MDMA-assisted psychotherapy more widely available to veterans could be life-changing for some. Current treatment for PTSD requires years of rigorous and difficult psychotherapy and medications that are prone to inefficacy, and there is an immense risk for veterans abandoning the process altogether as a result.
An unfortunate reality is that current and former members of the military affected by PTSD are at an increased risk for suicide, making it imperative to find effective treatments that are more swift and profound than what is currently available. MDMA-assisted psychotherapy seems to offer such hope.
Closing thoughts and resources
PTSD is a serious mental health condition that requires effective treatment and compassionate care. There is an urgent need to offer veterans more innovative solutions, and MDMA-assisted psychotherapy could offer treatment with an improved rate of success.
For more information about PTSD, resources are available from the National Institute of Mental Health and American Psychiatric Association.
If you or someone you know is struggling with symptoms of PTSD, it is important to contact a mental health professional as soon as possible. Do not wait for MDMA-assisted psychotherapy to become widely available, find help now. If you or someone you know feels unsafe or is experiencing suicidal ideation of any degree, call 911 or seek emergency medical attention immediately.