Medical Editor: Dr. Benjamin Malcolm, PharmD, MPH, BCPP
Contemplating the use of psychedelics alongside antidepressants? This guide about psychedelics and antidepressants explains the risks, benefits, and guidance you need to make informed decisions.
Why are people with treatment-resistant depression turning to psychedelics?
Have you ever felt like there’s this elephant in the room between you and your therapist or psychiatrist? Like they don’t want to give it to you straight, that what they’re offering as treatment just isn’t working like you hoped it would?
Sometimes medication and therapy can take too long to provide relief, let alone deep healing. Many don’t even have access to appropriate mental health care. High costs, insufficient insurance coverage, limited range of covered providers, and long waitlists are barriers to treatment for people who need it the most.
A person with depression may go through many providers, modalities, and medications in search of healing. Too many aren’t getting better. One study found that 10%–30% of patients with major depression either did not improve or demonstrated only a partial response when given antidepressant medication. Despite years of therapy and medication, many people still struggle with low mood and difficulty functioning, suicidal ideation and self-harm, and overall poor quality of life.
Furthermore, antidepressant medications such as SSRIs or SNRIs can come with acute and chronic side effects, including headaches, diarrhea, nausea, weight gain, anxiety, insomnia, dizziness, dry mouth, and sexual dysfunction. They need to be taken every day to be effective, and physical dependence occurs with long-term use which can lead to withdrawal syndromes and difficulty stopping their use.
Persons who don’t get better with several trials of antidepressants receive the diagnostic label of “treatment-resistant.” As different treatment options fail for these persons a sense of hopelessness about their situation can be exacerbated. Suicide is the second leading cause of death among individuals between the ages of 10 and 34 and the fourth leading cause of death among those between the ages of 35 and 54. There is an obvious and urgent need for more treatment options.
While still in its infancy, psychedelic-assisted therapy is showing promising evidence for treatment-resistant depression (TRD). Ketamine, a dissociative anesthetic with psychedelic properties, has yielded a 67% response rate in patients with treatment-resistant depression as well as rapid anti-suicidal effects. Most patients experience substantial relief within hours following administration. Traditional antidepressants take 2-6 weeks before they demonstrate an effect, so rapid effects are a major upside in comparison to standard treatments.
Ketamine is a schedule III controlled substance and is available for medical and psychiatric use in a range of healthcare settings across the US. The nasal spray Spravato (esketamine) is the only formulation of ketamine that is FDA-approved for treating depression. However, providers are free to prescribe ketamine ‘off-label’, which may include the use of ketamine by injection, infusion, or even sublingual lozenges. Due to ketamine producing psychedelic effects, treatment is likely optimized with therapy assisting its use, although not all practitioners provide ketamine-assisted psychotherapy. Standards of care written by ketamine providers state that supportive therapy is a core part of ethical use of ketamine for mental health purposes.
Psilocybin is another psychedelic medicine that’s showing promise in preliminary studies for TRD. Two studies have found that two treatment sessions resulted in significant symptom reduction that persisted from the start of therapy and continued through follow-up at six months. Investigators described the results as promising. “If supported by larger and better controlled trials, psilocybin’s low toxicity, favourable side effect profile and putative rapid and enduring antidepressant action could render it at least competitive with currently available treatments for major depression, whose therapeutic actions may be either delayed, e.g. in the cases of SSRIs and psychotherapy, or short-lived, e.g. in the case of ketamine.” The FDA has taken notice of the results, granting a “breakthrough therapy” designation to psilocybin for TRD to two seperate pharmaceutical companies due to the potential for significant advantages over existing therapies.
Let’s look at the neurobiological aspect of common antidepressants, psychedelics, and what it might look like to combine them.
How Common Antidepressants Work (SSRIs and SNRIs)
The most common types of traditional antidepressants are SSRIs and SNRIs, although there are other antidepressants that work similarly such as SPARIs and SARIs. SSRIs stands for selective serotonin reuptake inhibitor, while SNRI stands for serotonin norepinephrine reuptake inhibitor. These classes of antidepressants block the reuptake of serotonin, a chemical messenger (neurotransmitter) associated with mood regulation, happiness, sleep-wake cycles, memory, and attention. When the reuptake of serotonin is inhibited, serotonin stays in the space between neurons, known as the synapse, for longer. The boost in serotonin leads to long-term neuroadaptive changes that underlie the benefits when the medications work.
Citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), fluvoxamine (Luvox), paroxetine (Paxil), and sertraline (Zoloft) are all SSRIs. SNRIs block the reuptake of both serotonin and norepinephrine. Examples include duloxetine (Cymbalta), venlafaxine (Effexor), and desvenlafaxine (Pristiq). Serotonin partial agonists and reuptake inhibitors (SPARIs) are a newer class of antidepressants that also primarily function to block serotonin reuptake and include vilazodone (Viibryd) as well as vortioxetine (Trintellix). Trazodone (Desyrel) and nefazodone (Serzone) are older medications that are prescribed less frequently for depression, although also work to block serotonin reuptake as well as serotonin receptors (SARIs).
These medications may require some time before they take effect for most people. Some people experience relief within two weeks, whereas others do not notice an effect for 6-12 weeks.
People taking SSRIs and SNRIs could experience adaptive changes in the brain that result in increased tolerance for and ability to work with challenging emotions. If the medication can help them feel more balanced, then they may be able to make behavioral changes that support psychological health, derive more benefit from therapy, and navigate difficult situations with greater ease.
Antidepressant therapies are not about numbing emotion, although blunted emotion can be a side effect. Ideally, the medication brings about a change whereby the person can function better in their circumstances. In this zone, people should have access to both the reasoning mind and the emotional heart.
With the support of a therapist and when working from this regulated space, sometimes called a window of tolerance, the room can be made to process underlying trauma associated with their depression.
Some find that antidepressants blunt their emotions too much. They no longer feel things as strongly as they used to, and a sense of manageable, bland flatness settles in. Their resilience, ability to function in their life, and distress tolerance come at the cost of losing passion, joy, and the sense of being fully alive.
How psychedelics work on the brain
Like antidepressants, most psychedelics work on the neurotransmitter serotonin, however do so in different ways. The most common types of psychedelics include serotonin-based psychedelics, which can be broadly divided into tryptamines (LSD, psilocybin, DMT, 5-MeO-DMT) and phenethylamines (MDMA, mescaline). Though the specific neurological modes of action of various psychedelics depend on the drug used, there are commonalities. For example, both phenethylamine and tryptamine psychedelics are capable of directly stimulating serotonin 2A receptors. Psychedelics are ‘mind manifesting’ or ‘soul manifesting’ and have been described of non-specific amplifiers of emotional content and sensory information. They produce expansive mood states that run a vast gamut of possible emotions ranging from euphoria, spiritual ecstasy, and a strong sense of sacredness to paranoia, panic and a sense of dying (ego-dissolution).
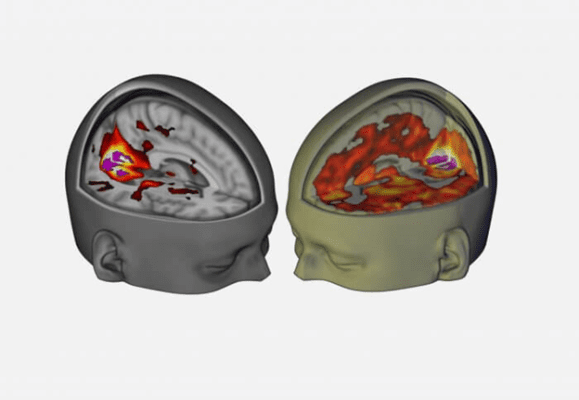
Neurological research indicates that the psychedelic experience increases the amount of disorganized activity across the brain as well as reduces activity of interconnected brain regions referred to as the default mode network (DMN).
This image from a study conducted by the Centre for Psychedelic Research at Imperial College London compares a placebo group on the left with a psilocybin group on the right. The study authors note, “This supports our idea that psilocybin disrupts the normal organization of the brain with the emergence of strong, topologically long-range functional connections that are not present in a normal state.”
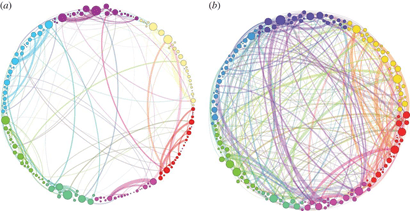
The same interconnectivity between disparate regions of the brain is also seen in LSD, as demonstrated by this graphic from the Beckley Foundation. The placebo group is on the left, and the LSD group is on the right.
By connecting disparate brain regions and reducing normal brain activity, such as those affiliated with the default mode network (DMN), psychedelics offer a non-ordinary state of consciousness with healing potential. The DMN is typically active when the brain is ‘at rest’ and is implicated in our sense of self and identity as well as rumination and negative beliefs common to depressive illnesses. By dampening this ingrained network, more expansive and less rigid views of the self can emerge, allowing for a rebuilding of identity and an opportunity to shift away from addictive behaviors and maladaptive coping mechanisms. Psychedelics increase neuroplasticity and can result in synaptogenesis or the formation of new neural connections. This may enable the individual to adapt, increase a sense of self-mastery or problem-solving abilities, and change the salience or emotional charges of traumatic memories.
How classic psychedelics, MDMA and ketamine work on the brain
While there are many similarities among various psychedelics, there are also differences in how they impact the brain as well as subjective experience, treatment settings, medical risks, and drug interaction profile with antidepressants. Many psychedelics appear to have ‘transdiagnostic potential’ or the ability to be effective for a range of psychiatric diagnoses. Critically important factors to successful therapeutic use beyond selection of psychedelic include the ‘set’ and ‘setting’ or mindset (therapeutic intention, preparation) and setting (support, physical environment, substance and dose). While research is still preliminary, response to psychedelics varies from person to person and certain psychedelics may have advantages for particular illnesses.
How does MDMA work?
MDMA-assisted therapy has the most evidence available for the treatment of PTSD. MDMA is a serotonergic amphetamine, meaning it has a higher risk profile for overdose and toxicity compared to psilocybin or LSD. The primary mechanism of action is around releasing serotonin into the synapse, although it can also bind serotonin 2A receptors. To a lesser extent MDMA releases norepinephrine and dopamine. It also has neurohormonal effects, such as release of the neuropeptide and social bonding chemical oxytocin that may be important to therapeutic effects. MDMA tends to lack hallucinogen effects and expands the emotional range without dissolving the ego.
How does Psilocybin work?
Psilocybin may be an effective intervention for anxiety in people with a terminal illness and is being studied for TRD, OCD, refractory headaches, eating disorders and more. It is considered a ‘classic psychedelic’ along with LSD and DMT. These serotonergic psychedelics mimic the action of serotonin closely and work primarily by binding serotonin 2A receptors. Psilocybin is a true hallucinogen and can produce ‘mystical experiences’ associated with almost complete ego-dissolution or loss of sense of self. This leads to a feeling of ineffable interconnectedness and oneness with all and is a powerful spiritual experience if it occurs.
How does Ayahuasca work?
Ayahuasca contains N,N-dimethyltryptamine (DMT) and harmala Monoamine Oxidase Inhibitors (MAOIs). The DMT is the psychedelic and works similarly to psilocybin and stimulates serotonin 2A receptors. The DMT experience is often characterized by an interaction with otherworldly or spiritual entities. Compared to psilocybin and LSD, DMT is also different because it does not build tolerance, thus ayahuasca is often consumed several nights in a row.
The MAOIs are important in making DMT work by mouth, although it introduces more risk for dangerous drug interactions with antidepressant medications compared to other psychedelics. Monoamine oxidase is a breakdown enzyme that works to metabolize neurotransmitters including serotonin. Use of MAOIs boost serotonin and reduce the ability of the body to metabolize it. When combined with other drugs that increase serotonin (SSRIs, SNRIs etc.), the presence of MAOIs increases the risk of physical toxicity such as serotonin syndrome.
Serotonin syndrome is a condition that can be thought of as serotonin poisoning with a range in severity levels. Many symptoms of mild serotonin syndrome overlap with normal ayahuasca experiences (e.g. diarrhea, dilated pupils, sweating or changes in body temperature, vomiting). However in severe cases, body temperature can increase to greater than 104.0 °F (40°C). Seizures, extreme muscle breakdown, respiratory failure and even death can occur when the wrong medications are mixed with ayahuasca.
How does Ketamine work?
Ketamine has antidepressant effects, although it works differently than both classic psychedelics and SSRIs or SNRIs. Instead of affecting one or more of the monoamine neurotransmitters (serotonin, norepinephrine, and dopamine), ketamine activates a different neurotransmitter called glutamate and is classified both as a psychedelic and dissociative. Because it does not work on serotonin, it has minimal interaction potential with regular antidepressants and can be used safely alongside them. For people experiencing suicidality and/or TRD treatment-resistant depression, ketamine has the most research supporting its use and is legally available. Ketamine has also been studied and found helpful for depression associated with bipolar disorders, which is generally considered a contraindication to serotonergic psychedelic use.
Can I take psychedelics while on antidepressants?
Few clinical studies have examined the effects of mixing psychedelics with antidepressants. However, understanding the mechanisms of action can allow scientists to make solid predictions about what may or may not be safe to do. Consulting with a knowledgeable professional before mixing antidepressants with psychedelics is recommended.
Persons taking antidepressants have reduced subjective experiences and worse outcomes in MDMA-assisted psychotherapy compared to persons that are not taking them. In fact, there may be an extended period of time after tapering and stopping antidepressants in which MDMA does not work as well. Interaction potential between MDMA and serotonin blocking antidepressants is more pronounced than with classic tryptamine psychedelics due to MDMA requiring the serotonin reuptake pump to release serotonin. While several clinical studies all suggest reduced effects of MDMA with antidepressants and have not resulted in adverse effects, other studies have found higher risks of death when combining MDMA with certain antidepressants. At this time, it appears persons may need 4 weeks or even longer for the full effects of MDMA to be restored after stopping antidepressants.
Serotonergic psychedelics such as psilocybin mushrooms, LSD, and DMT (without MAOIs) should all be safe to use while on antidepressants, although the antidepressant may dull some subjective effects. This effect appears somewhat inconsistent, particularly with psilocybin, raising questions about the necessity of tapering antidepressants prior to use. According to an interview with Dr. Ben Malcolm, clinical psychiatric pharmacist, the risks and complications of tapering off an antidepressant for some people may be more severe than taking the risks of a reduced psychedelic experience by combining psilocybin with antidepressants.
While ayahuasca does contain DMT, the MAOI components of ayahuasca create potential for dangerous drug interactions. It’s not safe to combine SSRIs, SNRIs, lithium or selected TCAs (tricyclic antidepressants) with ayahuasca because of the MAOI. These and other medications should be tapered down and completely discontinued before ayahuasca consumption. The period of time needed ranges depending on the antidepressant, but generally, two weeks or more is advised. It’s also not safe to combine ayahuasca with strong stimulants such as amphetamine or cocaine. For a full list of ayahuasca contraindications, read here.
Ketamine is safe to combine with antidepressants. In fact, Esketamine, a ketamine nasal spray, is indicated for TRD in conjunction with standard antidepressants can only be prescribed to someone who is taking an antidepressant already.
How to talk to your psychiatrist or find qualified alternative providers
If you are working with a prescriber such as a psychiatrist, nurse practitioner, or doctor, you may wish to have a conversation with them about psychedelic therapies, particularly if you’ve tried several antidepressants without getting adequate relief. Something as basic as, “Have you heard about the research into psilocybin for depression or MDMA for PTSD?” could be a good start.
Even though clinical trials show promise that psychedelics can address a range of mental health issues, medical professionals may be reluctant to endorse them due to stigma, legal status, or low amounts of high quality evidence.
Working with a provider who has knowledge of psychedelics might be a good idea if your prescriber won’t entertain the conversation or is unaware of the terrain. Psychedelic.support, the MAPS Integration Resource List, and Psychable all host a variety of providers who are knowledgeable of psychedelics. The Spirit Pharmacist has excellent educational resources and can be booked for individual consultations as well.
While there is still much to learn about antidepressants and psychedelics, it’s clear that given their overlap in working on serotonin and therapeutic potential in addressing mental illnesses that are traditionally managed with serotonin reuptake blocking antidepressants, this is an area of great importance when it comes to optimizing benefits and safety of psychedelic therapies.