Medical Editor: Dr. Benjamin Malcolm, PharmD, MPH, BCPP
Ibogaine for Addiction Treatment
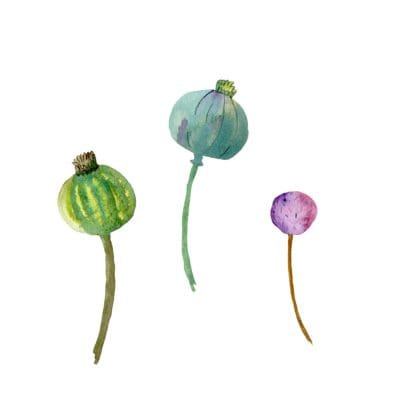
Ibogaine is most known for its ability to eliminate withdrawals from opiates and also for its intense, long, and vivid visionary journey. Ibogaine refers to the psychoactive indole alkaloid derived from the root bark of the West African perennial shrub Tabernanthe iboga, which is part of the Apocynaceae family. Traditionally used by Pygmy people, who shared its use with the Bwiti people of Gabon, the root bark is traditionally ingested for improving stamina on hunting excursions, to stave off fatigue, hunger, and thirst, and for some healing modalities. Most notably, large quantities are used for spiritual initiation into the Bwiti tribes.
Ibogaine hydrochloride can be extracted from the root bark of Tabernanthe iboga. Beyond its apparent ability to eliminate opioid withdrawals, it is reportedly profound at healing substance use disorders (SUD), commonly referred to as addiction.
There are many self-reports of withdrawal symptoms from substances such as heroin completely eliminated within one to two hours of ibogaine ingestion. Aside from eliminating withdrawal symptoms in opioid users, ibogaine also reduces drug cravings, potentially lowering the risk of continued drug use in individuals with dependencies on narcotics. In recent years, peer-reviewed journals have highlighted the benefits of using ibogaine to treat addiction to stimulants such as cocaine and methamphetamine, opioids, nicotine, and alcohol. Anecdotally, forums on the internet dedicated to discussing ibogaine claim it may work for other dependencies.
The World Health Organization (WHO) reports that 35 million people have a SUD, yet long-term treatment solutions are lacking. Ibogaine is an alternative treatment that has helped many, and the ones it has helped often become inspired about the possibility of it helping others.
It is important to remember that ibogaine alone is not a cure or ‘magic bullet’ for addiction and needs to be paired with proactive solutions for learning healthy coping mechanisms for long-term success. This can include integrating the ibogaine experience, engaging with addiction recovery and support therapies or programs, creating new behavioral patterns, addressing trauma, and other lifestyle changes that maintain or improve health.
Research on Ibogaine
Research regarding ibogaine pale compared to other psychedelics such as psilocybin and ketamine, possibly due to the fatalities associated with ibogaine and perception of being very dangerous and subjectively unpleasant. Still, we do have some research, and it’s promising.
Ibogaine and noribogaine have demonstrated positive effects in reducing the administration of addictive drugs including nicotine, alcohol, cocaine, and opioids in rodents. Inspired by the encouraging evidence from pre-clinical studies on animals, attempts to replicate ibogaine synthetically without the deadly and unpleasant side effects are underway. If the evidence continues to show a positive impact on substance use disorders, the addiction treatment world could be revolutionized by breakthroughs with ibogaine-assisted therapies or associated analogs.
Is an Ibogaine Trip Necessary to Treat Addiction?
Does it Have to Be Ibogaine?
In December 2020, a study was published describing a synthetic analog of ibogaine, without the cardiac risk and visionary side-effects. The analog showed a reduction in self-administration of alcohol and opioids and promising results for depression. Specifically, mice who had been trained to dose themselves with alcohol reduced consumption after a single dose of the ibogaine analog, called TBG. Another ibogaine analog, 18-mc, has the same anti-addictive properties but without the risks, unpleasant side-effects, and visionary experience.
Analogs such as TBG and 18-mc could change the western standard treatment model for addiction. In addition, the absence of the visionary experience changes the ibogaine treatment model. These analogs rely on the idea that the “trip” is unnecessary to long-lasting recovery, something many people are divided on.
On one hand, there is more experience in Gabon over the last 13,000 years than anything we have gathered anecdotally or scientifically in the western practice of ibogaine treatment. The lineage holders of this medicine rely heavily on teachings from the visionary state. Ibogaine providers around the world have seen clients receive life-changing epiphanies during their dream states. Some providers claim that unpleasant side-effects are necessary as people who have been using drugs need to learn how to sit with unpleasantness; they see value and healing during this time.
On the other hand, the risks of ibogaine treatment can be high, potentially fatal, and some people are not candidates for it to begin with. Lineage holders of ibogaine have no experience with analogs, making it hard to fully invest in the hypothetical necessity of ibogaine’s subjective effects for substance use disorder treatments. Whether the subjective effects or even use of ibogaine is necessary will remain a topic of high interest in addiction research for the near future.
Ibogaine and Alcohol Research
Alcohol is a sedative and neurotoxin that negatively affects the brain and body, specifically taxing on the brain and liver when used chronically in high doses. In alcohol use disorders, physical dependence can occur leading to severe withdrawals that can include medical risks such as seizures or delirium tremens. Due to the risk of seizures, ibogaine should only be given for alcohol dependency once the individual has detoxified from alcohol. Due to the dangers of alcohol withdrawal, this should be done in a medically supervised setting.
Ibogaine modulates and increases the neurotrophic factor GDNF in the brain, reducing cravings and aiding in post-acute withdrawals in alcohol-dependent people. Noribogaine, ibogaine’s metabolite that is long-lasting and has protracted benefits, is theorized to continue to reduce alcohol cravings and also alleviate depression. In a 2005 study that focused on ibogaine’s mechanism of action on GDNF and ethanol self-administration in rats, rats showed a dramatic decrease of ethanol intake immediately after ibogaine administration and also two weeks later, suggesting the potential for ibogaine as an effective treatment for alcohol. Long-term alcohol use disrupts the brain’s ability to produce dopamine and serotonin. There is some evidence that ibogaine can repair these systems.
Anecdotally, people who have gone to ibogaine treatment centers agree. The introspective and self-reflection that can occur during the dream-like state on ibogaine may also help people who are dependent on alcohol. It may help a person process trauma and events that may contribute to their alcohol use; it may also help a person create a path to move forward on.
Ibogaine and Cocaine Research
Cocaine is a central nervous system stimulant that produces large increases in dopamine in the brain. Prolonged use of cocaine changes the brain’s neurochemistry. Ibogaine’s mechanism of action with serotonin, dopamine, and the kappa receptors may play a part in its ability to help people with cocaine dependency.
In an observational study on humans, ibogaine reduced cocaine use as well as elevating mood, alleviating symptoms of depression, and other post-acute withdrawal symptoms, such as low energy. In studies on rodents, mice and rats continually decrease their self-administration of cocaine in studies. Among the ibogaine community, many providers and clients talk about a “resetting” process or a complete reset of tolerance from current dependencies. There is some evidence to suggest that neuroadaptation may occur with cocaine and methamphetamine.
Ibogaine has shown to be beneficial for the dampening of cravings that arise with cocaine cessation. Noribogaine, Ibogaine’s long-lasting metabolite, may help alleviate anhedonia and the depression that comes with post-acute withdrawal syndrome (PAWS).
There is scarce research on ibogaine and other stimulants, but one study on ibogaine and methamphetamine suggests that ibogaine works similarly with methamphetamine as it does cocaine. Substances such as cocaine, methamphetamine, amphetamine (Adderall, Vyvanse), and methylphenidate (Ritalin) need to be stopped for a period of time before working with ibogaine.
Ibogaine and Opioid Research
Ibogaine has a complex mechanism of action that is not fully understood yet. However, studies show promising results that ibogaine can decrease cravings, prevent relapse for an extended period of time, and lower self-reported feelings of depression. Both ibogaine and noribogaine bind to mu as well as other opioid receptor sites, although lack responses considered classic of opioids (e.g. pupil constriction, respiratory depression).
While noribogaine binds as an agonist at mu and kappa opioid receptor sites, ibogaine is not a heat-seeking missile: It works across multiple neurotransmitters. Combined effects across systems may be responsible for the interrupting of opioid withdrawals. Ibogaine also has a significant relationship with NMDA receptors. This relationship, as well as the modulating of GDNF and BDNF neurotrophic factors, may contribute to the promotion of neuroplasticity and “reset” feeling many people describe after ibogaine.
Research on opioid detoxification using ibogaine has primarily focused on heroin and morphine due to the need to be taking short-acting opioids to be a candidate for ibogaine therapy and the prevalence of heroin use disorder. Still, we can reasonably assume persons taking other short-acting opiates, such as oxycodone and hydromorphone, will react similarly to ibogaine. People who use opiates (morphine, heroin) only have to stop their opiate use for 9-12 hours before ibogaine treatment, unlike most other drugs, which require a number of days or weeks. Therefore, abstaining overnight for sleep is enough to proceed. Ibogaine has a profound resetting process with opiates, the individual’s tolerance is returned to a pre-dependent state, suggesting neuroadaptive properties. If there is a single substance ibogaine appears to seamlessly be made for, it’s short-acting opiates.
The use of long-acting opioid medications and synthetics used in the treatment of OUD such as methadone, fentanyl, and buprenorphine disqualify a person from using ibogaine. Persons using these medications or other long-acting opioids will be required to switch to short-acting opioids for successful detoxification and treatment of their OUD. Ibogaine treatment for opiate dependency eliminates nearly all withdrawal symptoms upon the first dosage and also significantly eliminates the possibility of Post-acute withdrawal syndrome (PAWS). If PAWS occurs, ibogaine booster doses help eliminate the symptoms.
Ibogaine and Nicotine Research
Nicotine is a highly addictive compound found in tobacco and smoking is a leading cause of preventable death. Nicotine quickly crosses the blood-brain barrier and agonizes the nicotinic acetylcholine receptor, leading to dopamine release and reinforcement. Once nicotine dependence is established withdrawal symptoms and cravings from nicotine set in quickly with cessation, increasing stress, and cravings. Ibogaine antagonizes Alpha-3-beta-4 receptors and inhibits acetylcholine receptors.
Studies have shown ibogaine to be effective for nicotine in dose-dependent amounts in rats. Rats were shown to reduce nicotine intake by up to 64% with ibogaine. However, the dosage of ibogaine mattered. Meaning, there is a threshold amount of ibogaine that seems to trigger the response necessary for nicotine cessation, and this threshold may be different in different people.
This coincides with anecdotal reports from ibogaine providers who have attempted to treat smokers. It may be worth noting that it is not common for smokers to seek out ibogaine for smoking alone. Usually, smokers have a primary reason for seeking out ibogaine treatment, something they are highly motivated to tackle that leads them to treatment. This may be why, anecdotally, reports from providers regarding nicotine are not as positive as studies have shown. The desire to quit has to come first.
Summary
Ibogaine is touted as a cure for addiction by many. However, anecdotal reports and limited research reveal a different reality. Unless proper aftercare and integration plans are put into place, relapse rates increase the farther away someone is away from their initial ibogaine treatment. Ibogaine is a catalyst for change. It is not a cure. Many experience life-changing revelations, profound transformation, and feel like a new person when they leave a treatment center. However, without hard work and dedication in learning how to live without the reasons that led them to treatment in the first place, old patterns may likely start to resurface.
Ibogaine also carries significant cardiac risk as well as other physical risks. Not everyone is a candidate for ibogaine treatment, and everyone interested should be thoroughly medically screened by their potential ibogaine treatment center. This is not a DIY substance and should always be used under the care of trained professionals. The research surrounding substance use disorder is promising, and anyone interested in ibogaine for addiction should vet their ibogaine center choices thoroughly.